Bacteria from meat could be causing more than half a million UTIs in the US every year, study estimates
(CNN) — Bacteria from meat could be responsible for more than half a million urinary tract infections in the United States every year, a new study says.
E. coli is an often-harmless bacteria that’s “part of the normal bacterial environment in the intestines in humans and animals,” said Dr. Craig Comiter, a professor of urology and obstetrics and gynecology at the Stanford University School of Medicine who was not involved in the new study.
Some strains can be dangerous, causing diarrhea, respiratory illness and pneumonia, according to the US Centers for Disease Control and Prevention.
Researchers have long known of a link between E. coli and UTIs, an infection in any part of the urinary system, including the kidneys, ureters, bladder and urethra; the bacteria causes 6 million to 8 million UTIs in the US every year.
But the new research suggests that more of these infections may be linked to E. coli from meat than previously known.
Infections can happen when meat with E. coli bacteria is not prepared with proper hygiene, passes through the digestive system and ultimately exits the anus. Because of its close proximity, that bacteria can easily enter the urinary system and cause an infection, with symptoms such as a burning feeling during urination, cloudy urine and pelvic pain.
Women have urinary tract infections up to 30 times more often than men do, according to the Office on Women’s Health.
What the study found
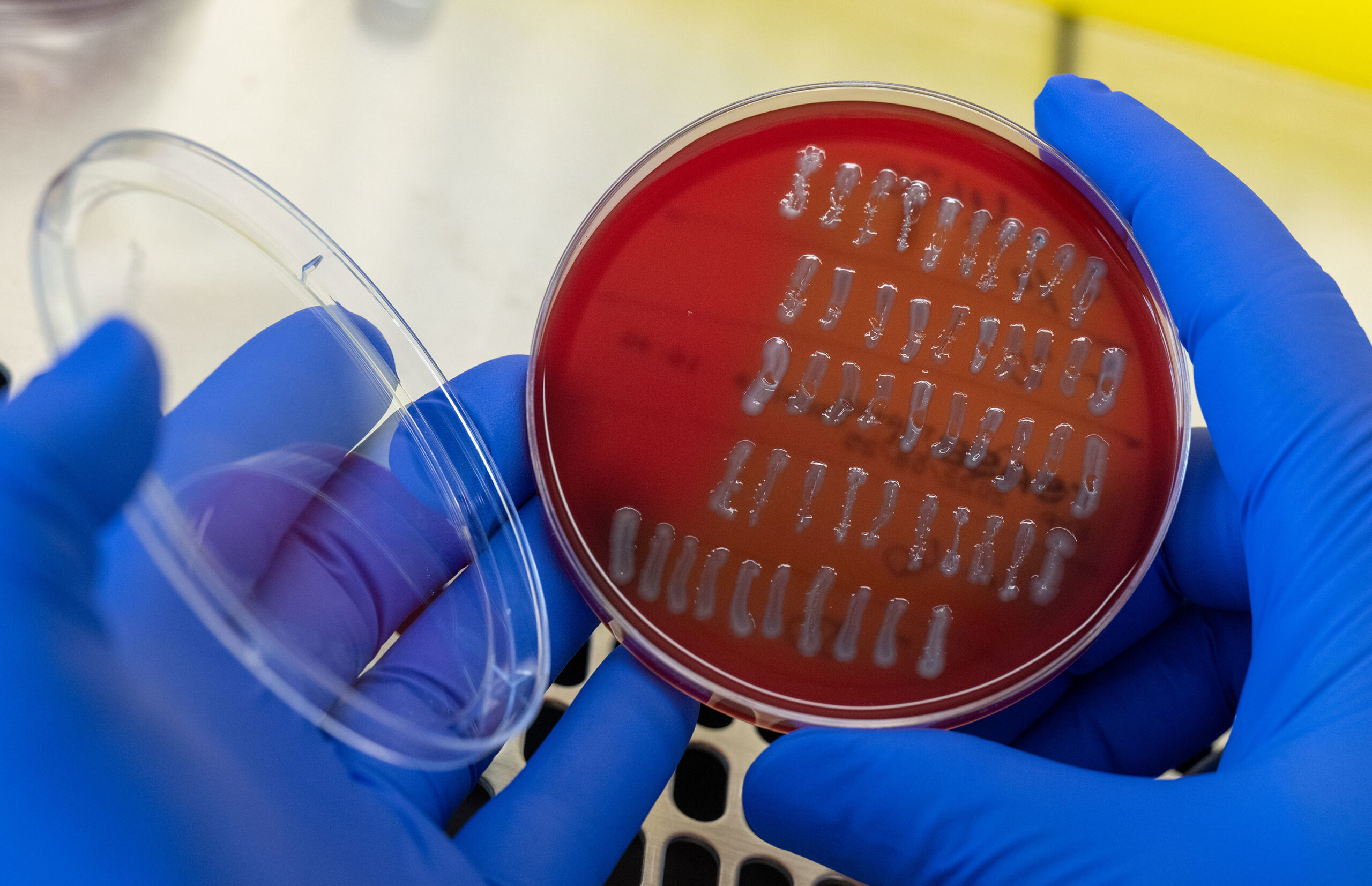
The study from George Washington University Milken Institute of Public Health analyzed data from retail meat samples collected between January 2012 and December 2012. The researchers looked at samples of chicken, turkey and pork from nine major grocery chains in Flagstaff, Arizona, and then took blood and urine samples from people hospitalized for urinary tract infections in the area at the same time.
It took 10 years to parse the data, including tracking the E. coli’s origins, said study co-author Dr. Lance Price, a professor of environmental and occupational health at George Washington University and the founder and co-director of the George Washington Antibiotic Resistance Action Center. But the dominant strains of E. coli present in 2012 remain the same now.
With the findings and a predictive model, the researchers estimated that 8% of E. coli urinary tract infections in the US each year — 480,000 to 640,000 cases — may be caused by strains from meat.
The researchers did not find that E. coli bacteria found in meat causes a greater rate of urinary tract infections; the findings simply explain why some infections might happen.
“It does not mean that if we didn’t have these bacteria, we’d have 8% fewer infections,” Comiter said.
If left untreated, urinary tract infections caused by E. coli can lead to problems like permanent kidney damage, sepsis and a narrowed urethra.
“Some people think of these as a painful annoyance … but they can actually be really serious infections because the bladder, the urinary tract, is actually a gateway to the blood,” Price said in a video released by George Washington University.
Once an infection is in the kidneys, it has access to the blood.
“The bladder is a major gateway to patients’ kidneys and bloodstream,” Dr. Cindy Liu, an author of the study and associate professor of environmental and occupational health at George Washington University, said in a news release.
Bloodstream infections are “super dangerous,” Price said, and those caused by E. coli kill 36,000 to 40,000 people a year in the US.
The researchers call for more monitoring of pathogens in raw meat found in grocery stores.
At home, people should be sure to wash hands when preparing or handling raw meat, and always use a separate surface to cook raw foods.
Understanding antibiotic resistance
The study findings also reveal another facet of the problem: the alarming rise of antibiotic-resistant infections. Most animals in the food industry are given antibiotics, but the overuse of antibiotics in animals breeds resistance, Comiter said.
Meat-associated bacteria is known to be especially resistant to treatment, he said.
“That is just the way animals are bred for food,” he said. “They’re going to pass infections to each other, so they need antibiotics so that they don’t die, so that we have a good source of protein.”
But resistant bacteria in meat can then passed along to the humans who eat it.
“As these bacteria become more and more resistant to antibiotics, there’s more infections that are progressing from the bladder, to the kidney, to the blood and, unfortunately, people are dying,” Price said.
Comiter believes that researchers should also focus on antibiotic use in animals.
“Perhaps we need to find a way to make burgers without giving the animals excessive antibiotics,” he said.