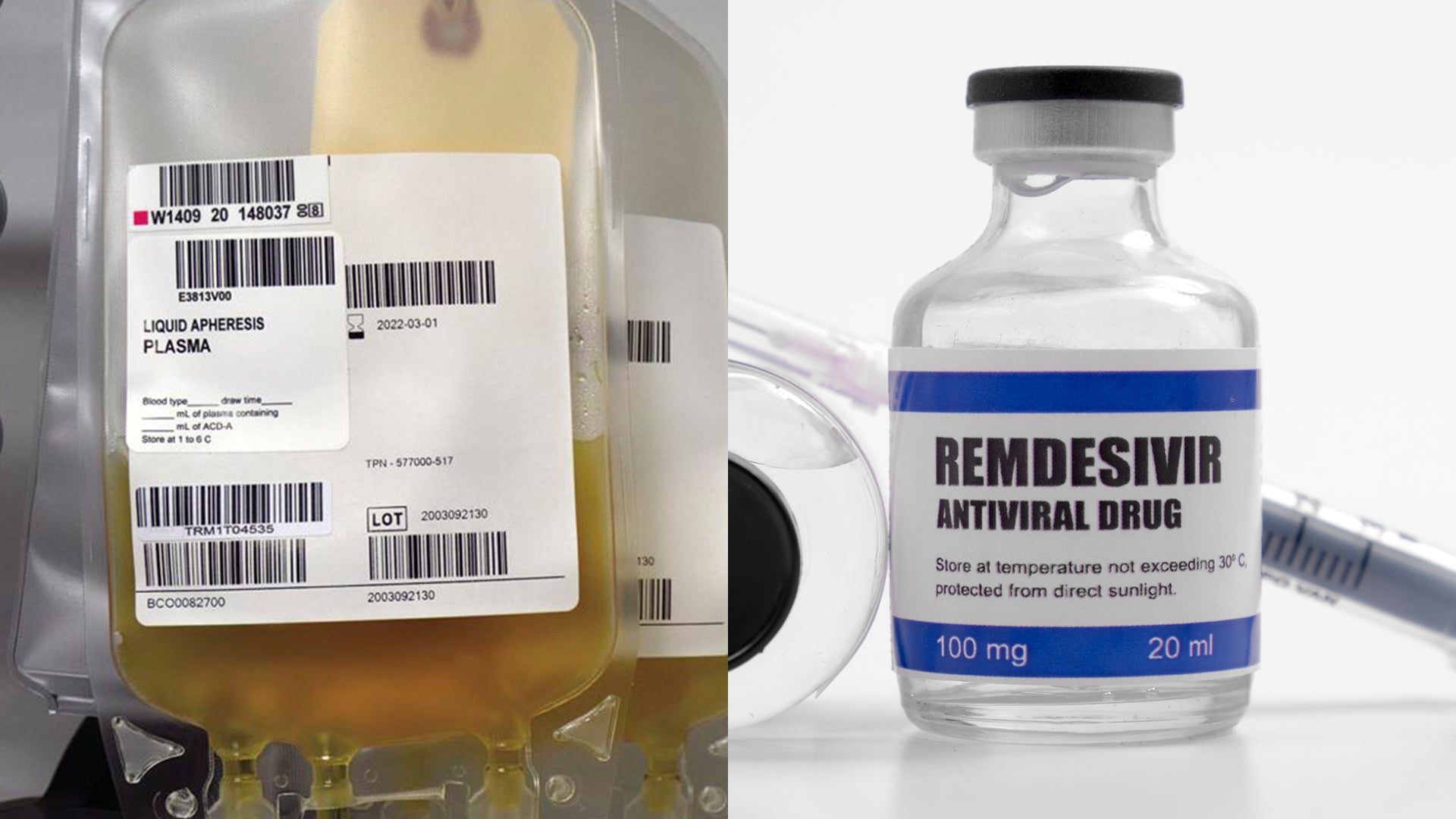
Convalescent plasma vs. anti-viral drugs: Does it warrant emergency use?
INDIANAPOLIS (WISH) – The Trump administration on Sunday announced an emergency use authorization for convalescent plasma.
This comes after months of testing on thousands of coronavirus patients with mostly positive results.
News 8 spoke with Dr. Christopher Doehring, vice president of medical affairs at Franciscan Health. Doehring spoke about the effectiveness of the treatment, how it compares to COVID-19 antiviral drugs and whether the method justifies the emergency use authorization.
Gillis: Can you explain what convalescent plasma is and how it aids in coronavirus recovery?
Doehring: In patients who’ve had COVID-19, their body’s immune system creates antibodies. So, convalescent plasma is pulling part of the blood that has the antibodies out of individuals and, in turn, giving it to other patients who have the coronavirus and may not have had an immune response just yet. So, it’s really taking advantage of immune protection from a patient who’s already been cured of their infection and offering it to someone who is in the early stages of their illness particularly if it’s severe.
Gillis: Is there a dose-response in terms of these antibodies that are given to coronavirus patients? Do we know of that yet?
Doehring: We don’t have that level of detail yet for COVID-19. We do use convalescent plasma in other types of infections when we need what’s called passive immunity by giving those antibodies. What we are learning about using convalescent plasma and COVID-19 is that some patients’ plasma have higher concentrations than others and the higher the antibody concentration the better and more effective it seems to be at reducing the risk of death.
Gillis: So, we know the quantity and concentration are important, but are some antibodies stronger than others?
Doehring: At this point, it’s a little premature to say. The virus itself has a number of different features to it. So, it’s almost as if one patient may develop one protein that protects from the virus while another person might develop another protein that might be more effective. But at this point it’s really about taking advantage of that generic response in someone who has been cured of their infection.
Gillis: I’ve heard these antibodies fade. How effective are they compared to other drug treatments such as remdesivir? And is this really a treatment or is this just buying us some time?
In some of these patients, a resulting immune response occurred and they have been cured. The Centers for Disease Control came out with a statement saying they can last about three months. We don’t know exactly how long their immunity will persist, but as far as the antibodies are concerned, there does seem like there is a limit to how long a person’s antibodies stay high enough to be able to continue donating. But we do know the higher the concentration of antibodies the better.
And like I said, the method is through passive immunity–when a newly infected patient hasn’t developed an immune response yet, so you’re taking advantage of the fact that someone else did. And it is a different mechanism than remdesivir. Remdesivir is an antiviral medication. So, you’re trying to attack the virus from multiple different directions by using these different treatments at this point.
Unfortunately, all of the things that we are using are still very early in terms of their trial phases and we’re still figuring out what works and what doesn’t. But certainly both remdesivir and convalescent plasma are showing some positive signs of helping to fight the virus.
Gillis: Is convalescent plasma something that warrants emergency use authorization?
Doehring: It’s been being used under a research protocol and so at this point we’ve treated tens of thousands of patients with convalescent plasma and there has actually been some pretty detailed analysis of the results so far. And I think under the circumstances given we don’t really have proven, compelling treatments yet what we know about convalescent plasma and the suggested benefit does seem to justify the emergency use autorization designation. This will then expand the availability of the convalescent plasma, too.
Gillis: What would you say to those who are hesitant to donate their plasma?
Doehring: Donating plasma is completely safe. There’s no issue. It doesn’t put a donor at risk. We’ve actually had a number of our own co-workers including several nurses who have become plasma donors. I think early on in this disease until we have more proven treatments it’s a tremendously sacrificial and patriotic thing to do to step up and donate. It could benefit someone you don’t know, which is something that is very admirable and doesn’t harm the donor in any shape or form.
News 8’s medical reporter, Dr. Mary Elizabeth Gillis, D.Ed., is a classically trained medical physiologist and biobehavioral research scientist. She has been a health, medical and science reporter for over 5 years. Her work has appeared in national media outlets. You can follow her on Instagram @reportergillis and Facebook @DrMaryGillis.