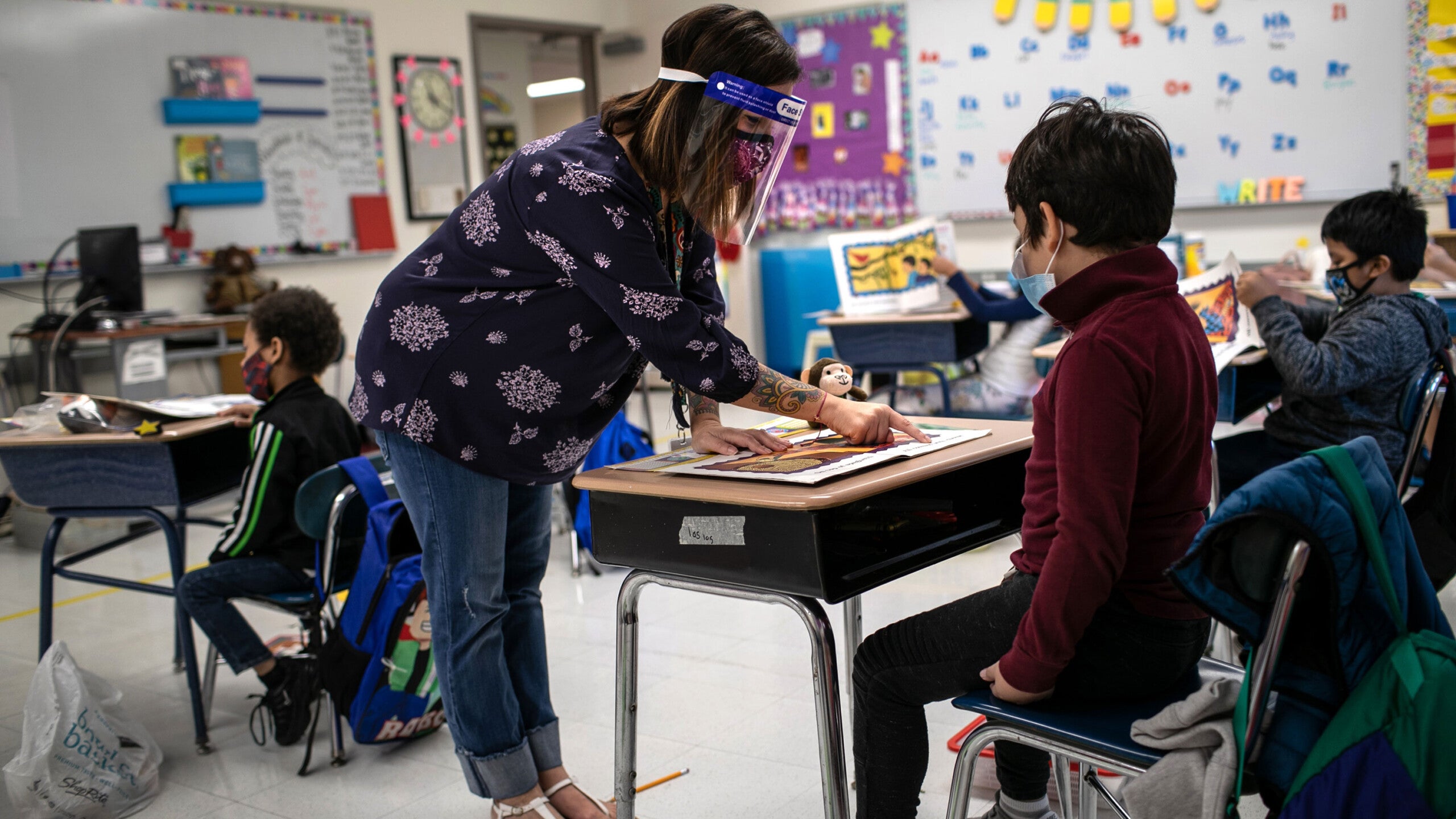
CDC must encourage better ventilation to stop coronavirus spread in schools, experts say
(CNN) — The U.S. Centers for Disease Control and Prevention should be doing more to guide and encourage improved air circulation in buildings — especially in schools — to help prevent the spread of coronavirus, ventilation experts say.
They say the CDC has not paid anywhere near enough attention to the role ventilation can play in helping the spread of coronavirus — or reducing it.
Schools will need to spend time and money improving airflow using heating, ventilation and air-conditioning (HVAC) systems, stand-alone high-efficiency particulate air-filtering (HEPA) systems or even just by opening windows if students, teachers and staff are to return safely to in-school learning in the fall, the experts say.
“The state of ventilation in schools in the United States right now is woefully inadequate,” Richard Corsi, dean of the College of Engineering and Computer Science at Portland State University, told a forum hosted by The Johns Hopkins Center for Health Security at the Bloomberg School of Public Health this week.
“Right now, schools are looking to CDC and they are not getting the answers to the kinds of things we are talking about,” Corsi added. “All of them look to CDC.”
Corsi said he has advised schools they need to improve ventilation, and their response has been that there is no specific guidance on the CDC website.
The CDC does suggest that schools think about ventilation improvements.
“Consider ventilation system upgrades or improvements and other steps to increase the delivery of clean air and dilute potential contaminants in the school. Obtain consultation from experienced Heating, Ventilation and Air Conditioning (HVAC) professionals when considering changes to HVAC systems and equipment,” it says in its guidance.
It also points to the guidance posted by the American Society of Heating, Refrigerating, and Air-Conditioning Engineers.
But that’s not enough, the experts agreed.
Why ventilation matters
With poor ventilation, viral particles can build up in the air in a classroom, cafeteria or hallway.
“If you look at all the high profile outbreaks — same underlying factors — no masks, low ventilation. It doesn’t matter if it’s spin class, ice hockey, camps, classrooms, choir practice or restaurants, (it’s) the same underlying factors,” Joseph Allen, who directs the Healthy Buildings Program at the Harvard T.H. Chan School of Public Health, told CNN earlier this month.
“The pandemic has revealed the role that our buildings, including schools, can play in infectious disease transmission,” William Bahnfleth, a professor of architectural engineering at the Pennsylvania State University, told the forum.
It’s a simple enough concept. People cough, sneeze or simply breathe out particles constantly. If a person is infected with a virus, including coronavirus, viral particles can be carried out on droplets that can become suspended in the air. In a closed room, those particles will build up and others will breathe them in.
The solution can also be simple — air exchange. Swap the particle-laden air for fresh, clean air, and the risk of transmission falls.
The problem comes when sealed buildings also have poor ventilation systems, and the problem is worse in colder months, when any windows or doors there might be are firmly closed against the chill.
Three full exchanges of air in a room can remove the infectious particles, Bahnfleth said. A high-performance air cleaning or ventilation system can do this in 20 minutes, he said.
“A portable HEPA system with a clean air delivery rate of 300 cubic feet a minute in a typical classroom gives you the equivalent of three to four air changes per hour. That, in many classrooms, is up to a 50%, 60%, 70% reduction in inhalation doses,” Corsi added.
But principals, school boards and teachers often know little about this concept.
“There is not a lot of awareness about indoor air,” said Claire Barnett, founder of the Healthy Schools Network. She said the problem has worsened since the U.S. Environmental Protection Agency stopped funding its indoor air program for schools 10 years ago. Neither CDC or the Department of Education has expertise on indoor air in schools now, she said.
And it’s a problem that, like so many others, affects poorer communities more.
“It’s been well documented for decades that the poorest communities often have the poorest school facilities. That means no clean air, no ventilation, nonworking plumbing, difficulties with sanitation leaks and molds,” Barnett said.
Bahnfleth pointed to a 2020 Government Accountability Office (GAO) study that found 54% of school districts needed multiple system updates. “About half of districts needed to update or replace multiple systems like heating, ventilation, and air conditioning (HVAC) or plumbing,” the report reads. “An estimated one-third of schools needed HVAC system updates.”
It costs money upfront, but it’s worth it, Bahnfleth said. “Yes, there may be significant costs involved in some cases, but not as high as some might think, and the cost of not making that investment is much higher,” he said.
So who should pay?
“There’s a need for investment, if only in filtering air cleaning systems for classrooms. This should be provided by the federal government,” Dr. Donald Milton, a professor of environmental health at the University of Maryland, told CNN.
There’s money for schools in President Joe Biden’s $1.9 trillion rescue plan, but none is earmarked for school ventilation systems.
And the CDC, he said, needs to do more to help people think about where the virus is — and that’s in the air.
“If it is in small particles floating in the air and you inhale them — it doesn’t matter how far it traveled in the air — the problem is the same. The solution is the same too: you need ventilation, filtration, and source control, and you need tight fitting masks with good filters and breathability,” he said.
What not to do
The experts advised against using unproven technology to “clean” the air, saying some approaches could result in contaminated air. The important thing is to exchange all the air in a room with fresh air several times an hour, they said.
“I want to implore everyone not to venture into unproven technologies that have slick marketing,” Corsi said during the Johns Hopkins forum.
That includes fogging or misting systems, disinfecting “robots” or on-the-spot ultraviolet light systems.
“Foggers and misters work ideally in certain settings,” Barnett said. They include laboratories or hospitals — not schools or office buildings where untrained workers have no idea how to use the dangerous chemicals involved.
Ultraviolet light systems that are installed high up in ceilings, with air circulation to take any breathed-out air up to them, work well, Bahnfleth said. But they can be expensive and are more appropriate for large, shared spaces such as gyms or cafeterias than small classrooms.
Some low-tech approaches can do more harm than good, also, said Barnett. Plastic shields, for instance, can concentrate contaminated air and may stop large droplets for a short period — think a grocery checkout — but are useless in settings such as classrooms where the air can circulate around them over time.
“If you can smell cigarette smoke from other side of the Plexiglass, you are also inhaling virus,” Barnett said.
All the experts were critical of the CDC’s emphasis on cleaning desks and others surfaces at the expense of the concept of clean air. “Surface cleaning isn’t very useful in terms of bang for the buck in Covid-19,” said Delphine Farmer, an aerosol expert at Colorado State University. If nothing else, cleaning solutions can fill the air with a complex cocktail of toxic chemicals, she said.
“There are very real consequences of overcleaning,” Farmer told the Johns Hopkins symposium.
The same applied to systems that use oxidative chemical processes to break down virus-laden particles.
“But in doing so they produce a series of organic compounds,” she said — including toxins such as formaldehyde.
“What we know works is ventilation and filtration,” Farmer said.