The truth about ‘patient zero’ and HIV’s origins
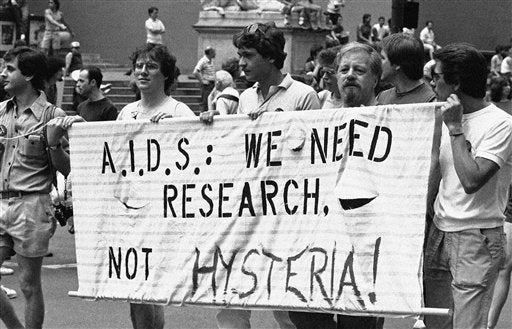
(CNN) — The man blamed for bringing HIV to the United States just had his name cleared.
New research has proved that Gaëtan Dugas, a French-Canadian flight attendant who was dubbed “patient zero,” did not spread HIV, the virus that causes AIDS, to the United States.
A cutting-edge analysis of blood samples from the 1970s offers new insight into how the virus spread to North America via the Caribbean from Africa. More than 1.2 million people in the United States currently live with HIV.
The research, conducted by an international team of scientists, was published this week in the journal Nature.
“No one should be blamed for the spread of a virus that no one even knew about, and how the virus moved from the Caribbean to the US in New York City in the 1970s is an open question,” co-author of the research, Dr. Michael Worobey, a professor and head of the ecology and evolutionary biology department at the University of Arizona, said at a news conference Tuesday.
“It could have been a person of any nationality. It could have even been blood products. A lot of blood products used in the United States in the 1970s actually came from Haiti,” he said. “What we’ve done here is try to get at the origins of the first cases of AIDS that were ever noticed. … When you step back in time, you see a very interesting pattern.”
‘Patient zero’ and the power of a name
In 1981, researchers at the Centers for Disease Control and Prevention first documented a mysterious disease. In their research, they linked the human immunodeficiency virus, or HIV, to sexual activity.
The researchers began to study one cluster of homosexual men with HIV, and beginning in California, they eventually connected more than 40 men in 10 American cities to this network.
Dugas was placed near the center of this cluster, and the researchers identified him as patient O, an abbreviation to indicate that he resided outside California.
However, the letter O was misinterpreted as a zero in the scientific literature. Once the media and the public noticed the name, the damage was done.
Dugas and his family were condemned for years. In Randy Shilts’ seminal book on the AIDS crisis, “And The Band Played On,” Dugas is referenced extensively and referred to as a “sociopath” with multiple sexual partners.
In 1987, the National Review referred to him as the “Columbus of AIDS,” and the New York Post called him “the man who gave us AIDS” on its front page.
“We were quite annoyed by that, because it was just simply wrong, but this doesn’t stop people from saying it, because it’s so appealing. You know, ‘The man who brought us AIDS.’ Well, if it were true, it would be annoying, but since it isn’t true, it’s even more annoying,” said Dr. James Curran, dean of Emory University’s Rollins School of Public Health and co-director of the university’s Center for AIDS Research.
Curran, who was not involved in the new research, coordinated the AIDS task force at the CDC in 1981 and then led the HIV/AIDS division until 1995.
“The CDC never said that he was patient zero and that he was the first person,” Curran said of Dugas.
“In addition to the potential damage to his reputation, it was also a damage to scientific plausibility. That there would be a single-point source to start the epidemic in the United States is not very likely. It’s more likely that several people were infected,” Curran said. “I think that the concept of patient zero has always been wrong and flawed, and scientists never said it.”
Dugas died in 1984 of AIDS-related complications. Now, more than 30 years later, scientists have used samples of his blood to clear his name.
Going back in time with blood
For the new research, Worobey and his colleagues gathered archival blood samples in New York and San Francisco that were originally collected for a hepatitis B study in 1978 and 1979. The samples came from men who had sex with men.
The researchers screened the samples and noticed that “the prevalence of HIV positivity in these early samples from hepatitis B patients is really quite high,” Worobey said Tuesday.
From the samples, the researchers recovered eight genome sequences of HIV, representing the oldest genomes of the virus in North America. They also recovered the HIV genome from Dugas’ blood sample.
As many of the samples had degraded over time, Worobey’s lab developed a technique called “RNA jackhammering” to recover the genetic material.
The technique involves breaking down the human genomes found in the blood and then extracting the RNA of HIV to recover genetic data about the virus, an approach that’s similar to what has been used to reconstruct the ancient genome of Neanderthals in separate studies.
“The major contribution which interested me the most was their capacity to restore full sequence genomes from very old serum samples using the jackhammer technique,” Curran said of the new research.
After analyzing the genomes, the researchers found no biological evidence that Dugas was the primary case that brought HIV to the United States, and the genome from Dugas appeared typical of the other strains already in the United States at the time.
The researchers discovered strong evidence that the virus emerged in the United States from a pre-existing Caribbean epidemic in or around 1970.
How HIV arrived in the United States
Sequencing genomes allows scientists to take a peek back in time to determine how a virus emerged and where it traveled by examining how many mutations appear in the genome.
Scientists estimate that HIV was transmitting in humans after a chimpanzee infected a single person sometime in the early 20th century in sub-Saharan Africa. The general consensus among scientists is that HIV then crossed the Atlantic and quickly spread through the Caribbean before it arrived in the United States, probably from Haiti, Curran said.
Scientists at the University of Oxford published a separate study in June suggesting that HIV spread through specific migration routes — based on tourism and trade — throughout the past 50 years as it made its way around the world.
The research team behind the new genetic analysis now hopes that its findings may lead to a better understanding of how HIV moved through populations — and how blaming a single patient for the pathogen’s rise remains troublesome.
“In many ways, the historical evidence has been pointing toward the fallacy of this particular notion of patient zero for decades,” Richard McKay, a historian of medicine at the University of Cambridge and a co-author of the new research, said at Tuesday’s news conference.
“The study shines light from different angles to better understand the complexity of an important period in the past,” he said. “In view of this complexity, one of the dangers of focusing on a single patient zero when discussing the early phases of an epidemic is that we risk obscuring important, structural factors that might contribute to its development: poverty, legal and cultural inequalities, barriers to health care and education. These important determinants risk being overlooked.”
CNN’s Ben Westcott and Emily Smith contributed to this report.